By Dr. Nicole Sundene
PCOS or Polycystic ovarian syndrome is a common Women's Health Hormone condition that is improved best by working with a Naturopathic Doctor in my humble opinion after twenty three years of experience working in both prescription and natural Women's Health.
My treatment for PCOS patients as a Holistic Hormone Doctor almost never require medications or birth control pills. There are alternatives to birth control pills and medications for PCOS patients that we will discuss today as well as the risks vs the benefits of many common medications prescribed for PCOS.
PCOS causes hormonal imbalance such as the disruption of estrogen, testosterone, DHEA, cortisol, and progesterone levels. As a result, various clinical symptoms develop, including PMS, Estrogen Dominance, abnormal heavy periods, irregular periods, no period or amenorrhea, anemia, infertility, and a high risk for cancer of the breast, uterus and ovaries when the hormone imbalance is left untreated.[1, 4, 7]
PCOS is common among women of childbearing years, between 15 to 44 years of age. PCOS is affecting 6% to 12% of US women aged between 15–49 years. A research study estimated the worldwide prevalence of PCOS between 6% and 26%. Women with a family history of PCOS or who have diabetes, insulin resistance, or obesity are at higher risk of developing PCOS. [1, 2]
Symptoms of PCOS
PCOS symptoms vary from mild to severe and mostly appear in the late teens or early 20s. It involves a few or many of the below symptoms. [1, 3, 7, 8]
Types of PCOS
Research studies categorized PCOS into many types based on the clinical symptoms and causes responsible for the development and progression. While mainstream prescription medicine manages all PCOS patients with oral birth control pills, metformin and spironolactone, these treatments often fail when we do not have the correct treatment for the correct type of PCOS. Determining which category of PCOS the patient falls in should be done first and foremost prior to implementing any PCOS treatments. The main PCOS types include: [8, 9]
New research on PCOS presented the following subgroups of PCOS patients based on genetic markers. [8, 9]
PCOS Diagnosis and its Criteria
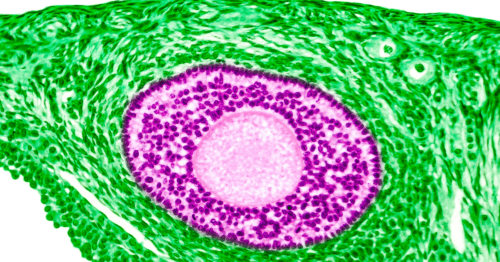
Diagnosis of PCOS should begin with the patient's questioning, family history, physical examination, and checking the other endocrine parameters. As PCOS is a complex disease, so research studies devised criteria for its diagnosis; based on the presence of hyperandrogenism, ovulatory dysfunction, and polycystic ovaries. The presences of any two clinical symptoms in the patient among the hyperandrogenism, ovulatory dysfunction, and polycystic ovaries are necessary for PCOS diagnosis. [2, 3]
The clinician should consider the menstrual history, weight gain or loss, and cutaneous findings such as excessive hair, acne, alopecia, and dark patches for hyperandrogenism confirmation. Plus, ask and evaluate the presence of ovulatory dysfunction via oligomenorrhea and amenorrhea. Also, check for the other medical complications associated with PCOS. [3]
Other lab approaches to assist the diagnostic criteria to include; [2, 3]
Medical Complications of PCOS
Women with PCOS are at high risk of developing certain medical complications. These include type 2 diabetes, gestational diabetes, heart disease, hypertension, depression, sleep disorders, eating disorders, anxiety, plaque formation, and stroke. [6]
PCOS Treatment Guidelines
Although there is no definite cure for PCOS; however certain kinds of treatment interventions are recommended for resolving PCOS symptoms and complications. These interventions include both pharmacological and non-pharmacological approaches that treat symptoms and regulate normal physiological function. While I do not recommend or prescribe pharmaceuticals for PCOS and do not personally find them effective for managing this condition as a female hormone specialist, I will still discuss the risks and benefits of medications for PCOS. [1, 2, 5]
Non-Pharmacological approach
Non-pharmacological approaches involve applying electrolysis that passes electric current into the hair follicles, damage them, and arrests hirsutism. [3]
Weight loss
Weight loss is considered a gold standard for managing PCOS symptoms as weight loss improves insulin sensitivity, particularly in obese PCOS women. Also, obesity increases the risk of metabolic and reproductive abnormalities associated with PCOS. Weight loss is recommended as the first line of treatment for infertility in obese women with PCOS. Unfortunately, there is no approach for permanent weight loss, and weight decrease relapsed in around 90-95% of patients. However, bariatric surgery significantly sustains and reduces weight in obese individuals. Moreover, a hypocaloric diet also helps weight reduction in women with PCOS. But there is no clear evidence of the positive impact of weight reduction on PCOS symptoms. [2, 3]
Natural Diet & Lifestyle For PCOS Symptoms
PCOS Medication Treatment
Different classes of medicines are used for the treatment of PCOS complaints. These include;
Metformin: It is an oral anti-diabetic medication that improves insulin resistance and decreases insulin concentration. Mostly, it is recommended as a second-line drug of choice after clomiphene that induces ovulation, lowers serum androgen, and helps menstrual frequency. Moreover, it showed the best results in combination with clomiphene in obese women with PCOS. Side effects associated with the use of metformin include lactic acidosis and gastrointestinal symptoms such as diarrhea, nausea, vomiting, abdominal bloating, flatulence, and anorexia. [1-3, 5]
Oral contraceptives: Oral contraceptives such as estrogen and progestin therapy help treat PCOS symptoms via inhibition of Luteinizing and androgen hormone secretion, increasing the Sex hormone-binding globulin level, and also act as steroids receptors blocker. The side effects of oral contraceptives include a high risk of thromboembolic events, developing type 2 diabetes, elevated cholesterol and triglyceride level, and may impair insulin sensitivity. Therefore a low dose of oral contraceptives is recommended as the above adverse events are high dose-dependent in high-risk women with PCOS. [1-3, 5]
Progesterone therapy: Natural progesterone and synthetic progesterone such as Cyproterone acetate and drospirenone provide anti-androgenic properties. Some women with PCOS may need a combination or natural progesterone with an oral contraceptive to treat PCOS. The side effects of progesterone therapy include mood elevation or depression, weight gain, and abnormal periods, heavy bleeding, cramping, and spotting. [1-3, 5]
Spironolactone: It helps the treatment of excessive hair and acne. However, there are limited studies about its effectiveness. It is advised to use it with caution in women with renal impairment as it aggravates hyperkalemia as a side effect. Also, it is not recommended during pregnancy due to teratogenicity (congenital disabilities). [1-3, 5]
Please Note: If you do not want to take medications for PCOS and prefer a nutrition and herbal medicine approach then you will be a perfect fit for treating your PCOS. Otherwise, the medicine I use to treat PCOS is nutrition changes, supplements and herbs so there is no point in signing up to work with me if you or your teenager are not willing to make dietary changes. I understand they are hard to do and struggle with them myself, but we at least need to be comitted to making these changes gradually over time to be successful with Naturopathy when treating PCOS symptoms.
If you think you will be able to use Naturopathy and need help diagnosing or treating your PCOS symptoms simply pop over to my SCHEDULE page to treat yourself to a Naturopathic visit!
Dr. Nicole Sundene, NMD
Dr. Sundene is a Naturopathic Doctor in Scottsdale, Arizona, and is considered a Female Hormone Expert in Women's Health and Bioidentical Hormones. She specializes in Holistic Women's Health for Menopause, Thyroid, Hashimotos, PMS, Perimenopause, Autoimmune, Postpartum, Chronic Fatigue, Depression, Anxiety, Food Allergies, Digestion, Dermatology , Acne, Psoriasis, Eczema and Adrenal Hormonal Conditions. In 1999 she began working for a Hormone Doctor prior to starting Naturopathic Medical School. With over 22 years of experience in both Prescription and Natural women's health and hormones she presents to women the best integrated health solutions for their Chronic Disease. She has been an Herbalist for over 27 years and enjoys teaching women how to use herbs to balance their hormones, nutrition and optimize their health. Dr. Sundene relies on blood testing for her hormone metrics. The hormone testing is covered per the patient's insurance plan and conducted at certain points in the woman's menstrual cycle. To learn more about Hormone Testing for Women Visit: Bioidentical Hormones. Follow Dr. Sundene on Instagram, Twitter and Facebook for more tips on Women's Health, Female Hormones and Naturopathy!
References



I am down 75 pounds as of today. I have never been able to lose weight with my PCOS until I found you and started Naturopathy. Thank you for your help! Stay Safe!
Cathy
Thank you for explaining why I need to work eating more protein for my PCOS. I know you keep telling me to eat more protein but I just hate meat and protein drinks. I have been using a lot more nut butters and nuts after reading this and do like that pea protein powder protein. It does taste good. God Bless you Doc!
The zinc has been such an amazing tip! I know you wanted me on it for my immune system but its nice seeing that it also is good for PCOS hair loss. This explains why my hair has been so much thicker since coming to see you.
Great information and this explains to me why so many doctors have told me "You can't have PCOS because you are too skinny. I have always had a hard time putting on weight because of a fast metabolism. Other than my weight everyone has told me I have all the symptoms of PCOS so it makes sense that there are different sub types. Thank you for offering women something other than Metformin for their PCOS. That is all I have ever been given and I am much better with your hormone program.
Life without Metformin is so much better. It was always making my stomach upset and actually was making me gain weight. Horrible drug. Naturopathic Medicine FTW!